SimplyPERIO™
Periodontal disease (also called gum disease) and its two stages, gingivitis and periodontitis, are inflammatory diseases triggered by pathogenic bacteria that lead to damage of the soft tissue and bone supporting the teeth. Periodontal disease is the most undiagnosed & untreated disease with the highest impact to so many bodily systems & functions.
Grounded in evidence-based research, the SimplyPERIO™ saliva test integrates the best available science from leading oral health experts into your practice for more clinically relevant treatment applications.
Only single test with the most complete multi-organism detection capability for all keystone periodontal and systemic oral health pathogens.
CAP/CLIA accredited testing laboratory
Physician ordered testing
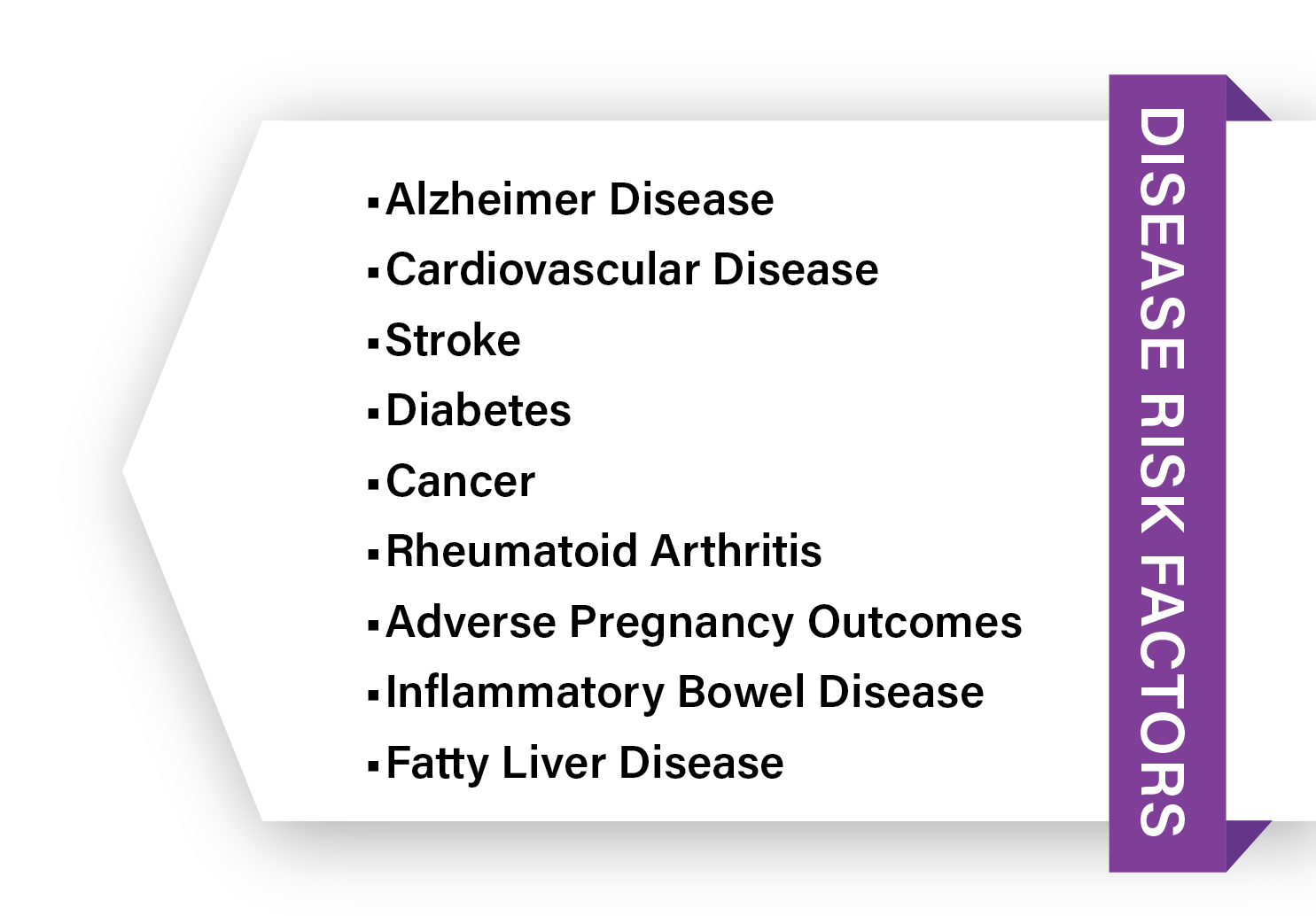
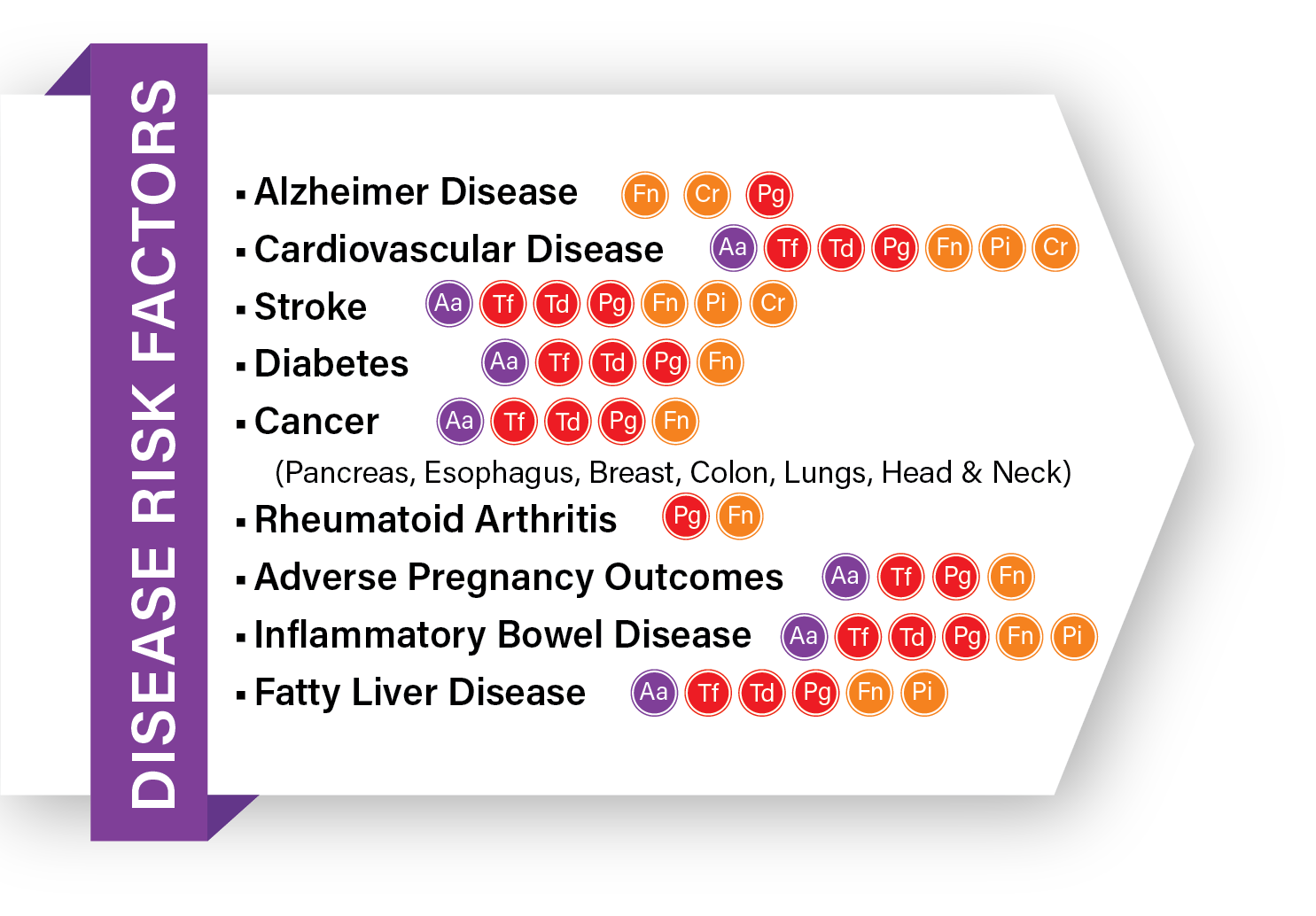
Assesses periodontal disease, organisms, and agents associated with systemic health issues.
Tests for Caries risk and Candida Albicans (Known to accelerate oral disease growth & progression.)
Screens for viral targets associated with cognitive decline.
Noninvasive, pain-free saliva specimen collection
Patented saliva preservation buffer holds, suspends, & stabilizes oral bioflora bloom at room temperature.
Most accurate target analysis eliminating sample overgrowth and cold chain storage hassle.
- Consistent, highly accurate, & dependable molecular testing
Intelligent health measures, real clinical relevance, & actionable clinical insights
Support at-home patient testing for follow-ups & treatment monitoring.
Results in 24-48 hours after received at the lab
Male or Female
Free Shipping
Purple Complex:
– Aggregatibacter Actinomycetemcomitans (AA)
Red Complex:
– Porphyromonas Gingivalis (Pg)
– Tannerella Forsythia (Tf)
– Treponema Denticola (Td)
Orange Complex:
– Prevotella Intermedia (Pi)
– Campylobacter Rectus (Cr)
– Fusobacterium Nucleatum (Fn)
– Fusobacterium Animalis (Fa)
Green Complex:
– Eikenella Corrodens (Ec)
Caries:
– Streptococcus Mutans (Sm)
– Streptococcus Sanguinis* (Ss)
Yeast:
– Candida Albicans (Ca)
*The presence of Streptococcus Sanguinis is associated with healthy plaque biofilm.
WHY TEST?
In some it may be easy to spot, however, in the vast majority, there may be dangerous and damaging periodontal disease pathogens hiding that can’t be identified by a perio probe or a visual exam. There are around 200-300 bacterial species residing inside the mouth. Out of this happy colonization, only a select few of these residents are contributors to dental decay (caries) or periodontal disease.
Testing delivers evidence of the presence of damaging levels of periodontal bacteria and drives more patients into the necessary periodontal therapy and better home care regimens they need. In addition, education from testing provides more dedicated patients signing up and committed to in-office oral healthcare regimens.
In some it may be easy to spot, however, in the vast majority there may be dangerous and damaging periodontal disease pathogens hiding that can’t be identified by a perio probe or a visual exam.
Testing delivers evidence of the presence of damaging levels of periodontal bacteria and drives more patients into the necessary periodontal therapy and better home care regimens they need. In addition, education from testing provides more dedicated patients signing up and committed to in-office oral healthcare regimens.



HAS SOME FORM OF GUM DISEASE






[1] https://www.ncbi.nlm.nih.gov/books/NBK554590/
[2] Pessi T, Karhunen V, Karjalainen PP, et al. Bacterial signatures in thrombosis aspirates of patients with myocardial infarction. Circulation. 2013;127(11):1219-1228. doi:10.1161/CIRCULATIONAHA.112.001254
[3] Freire MO, Van Dyke TE. The mechanisms behind oral-systemic interactions. In: Glick M, ed. The Oral-Systemic Health Connection: A Guide to Patient Care. Chicago, IL: Quintessence; 2014:Chapter 5, 103-119.
[4] Leishman SJ, Do HL, Ford PJ. Cardiovascular disease and the role of oral bacteria. J Oral Microbiol. 2010; 2. doi: 10.3402/jom.v2i0.5781.
[5] Karpiński T. M. (2019). Role of Oral Microbiota in Cancer Development. Microorganisms, 7(1), 20. https://doi.org/10.3390/microorganisms7010020
WHO
TO TEST?
- Test everyone! (Periodontal disease is the most undiagnosed & untreated disease with the highest impact on so many bodily systems and functions.)
- Patients with bleeding (Gingivitis) while charting or cleaning and those with mild, moderate, or severe Periodontitis.
- Those patients with unexplained inflammatory biomarkers such as hsCRP.
- All patients’ pre and post-restorative care procedures (braces, extraction, root canals, implants).
- Those currently pregnant or actively pursuing pregnancy.
- All patients at current risk of any systemic health disease.










Periodontitis
Periodontitis
Periodontitis
Periodontitis




(Biofilm)
Bacterial Infection
Reduction
Increased Risk for Other
Medical Complications


FAQ’s
Frequently Asked Questions
A recent analysis led by National Institute on Aging (NIA) scientists suggests that the bacteria associated with periodontal disease that causes the chronic inflammation are also associated with the development of Alzheimer’s disease and related dementias, especially vascular dementia.
A new study finds an association between tooth loss, gum disease (or periodontal disease), and a shrinking of the brain area thought to be involved in memory, and specifically with Alzheimer’s disease. Brain volume is an indicator of atrophy and loss of cognitive function that can occur with age or disease. According to the study, a missing tooth was the equivalent of brain shrinkage of nearly an additional year of brain aging, and severe gum disease was equal to 1.3 years of brain aging.
—
https://www.medicalnewstoday.com/articles/poor-dental-health-may-increase-alzheimers-risk
https://www.nia.nih.gov/news/large-study-links-gum-disease-dementia
https://www.nia.nih.gov/news/tooth-loss-older-adults-linked-higher-risk-dementia
https://www.washingtonpost.com/wellness/2023/09/21/teeth-gums-oral-health-dementia-alzheimers/
Stillbirth is a significant public health concern, accounting for 60% of perinatal deaths. Infections account for 10–25% of all stillbirths. Study demonstrates Fusobacterium nucleatum (Fn) from the mother’s oral cavity found in post mortum examination of stillborn baby.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3004155/
https://www.sciencedaily.com/releases/2010/01/100121171411.htm
Compared with people who have healthy gums, people with periodontal disease are about twice as likely to have a heart attack. (https://www.health.harvard.edu/heart-health/gum-disease-and-heart-health-probing-the-link)
According to the experts at Harvard, people with gum disease (also known as periodontal disease) have two to three times the risk of having a heart attack, stroke, or other serious cardiovascular event. And according to the American Heart Association, adults with periodontitis, a severe gum infection, may be significantly more likely to have higher blood pressure compared to individuals who had healthy gums.
Pathogens that can have an impact on cancer development in the gastrointestinal tract are also found in the oral cavity. People who have periodontal (gum) disease may have a higher risk of developing some forms of cancer, suggests a letter published in the journal Gut detailing a prospective study. US researchers found that a history of periodontal disease appeared to be associated with a raised risk of oesophageal (gullet) cancer and gastric (stomach) cancer and this risk was also higher among people who had lost teeth previously.
Previous findings on the relationship of periodontal disease and tooth loss with oesophageal and gastric cancer have been inconsistent. Therefore, a team of researchers from Harvard T.H. Chan School of Public Health, in Boston, USA, carried out a study of data on patients over decades of follow up. They examined the association of history of periodontal disease and tooth loss with the risk of oesophageal and gastric cancer in 98,459 women from the Nurses’ Health Study (1992–2014) and 49,685 men from the Health Professionals Follow-up Study (1988–2016).
The results showed that during 22–28 years of follow-up, there were 199 cases of oesophageal cancer and 238 cases of gastric cancer. A history of periodontal disease was associated with a 43% and 52% increased risk of oesophageal cancer and gastric cancer, respectively.
—
https://www.bmj.com/company/newsroom/gum-disease-may-raise-risk-of-some-cancers/
A new peer-reviewed BaleDoneen study is the first to reveal a new, treatable cause of cardiovascular disease (CVD): periodontal (gum) disease due to certain high-risk oral bacteria. The research was published in the April issue of Postgraduate Medical Journal (PMJ).
The oral-systemic connection is the link between the health of your mouth and your overall health. A landmark 1954 study was the first to show that oral germs, such as those that cause gum disease, frequently enter the bloodstream and quickly spread throughout the body. Among the ways this can happen are through periodontal cleaning, tooth extractions, tooth brushing, and even chewing food.
The spread of these germs throughout the body can result in chronic inflammation, a fiery process linked to many disorders, including cardiovascular disease (CVD, also known as heart disease), diabetes and even some forms of cancer. Poor oral health has also been linked to dementia, rheumatoid arthritis and even pregnancy complications, according to the American Academy for Oral Systemic Health.
Research suggests that the harmful cardiovascular effects of PD are due to a few high-risk oral bacteria discussed in the BaleDoneen study: Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola or Fusobacterium nucleatum.
Studies show that CVD results from a triple whammy known as the atherosclerotic triad. (Atherosclerosis is plaque buildup in the arteries that can lead to a heart attack or stroke.) The BaleDoneen study is the first to show that these bacterial villains can intensify each component of the arterial disease-inducing triad, creating a perfect storm of harmful effects, as follows:
- People with gum disease have up to twice as much small, dense LDL cholesterol (the most dangerous kind) in their blood as those with healthy gums, according to a recent study. The size of cholesterol particles matters: Some are big and buoyant, so they tend to bounce off vessel walls, while others are small and dense, making it easier for them to penetrate the arterial lining. Think of the difference between beach balls and bullets.
- Chemicals produced by high-risk oral bacteria make the walls of the artery more permeable, so it’s easier for bad cholesterol to invade. Since people with PD due to these pathogens also have higher blood concentrations of small, dense LDL cholesterol, and other disease-causing lipoproteins, this creates a one-two punch on the arteries, much like a gang assault on a house with broken windows or doors.
- Substances produced by high-risk bacteria can also make the inner layers of the arterial wall (where plaque forms) stickier, much like Velcro, so bad cholesterol is more likely to get trapped there and create plaque deposits, resulting in a triple threat to arterial health.
Read more here: https://baledoneen.com/blog/the-oral-systemic-connection-how-bacteria-in-your-mouth-can-harm-your-heart/
—
Additional Sources:
Pessi T, Karhunen V, Karjalainen PP, et al. Bacterial signatures in thrombosis aspirates of patients with myocardial infarction. Circulation. 2013;127(11):1219-1228. doi:10.1161/CIRCULATIONAHA.112.001254
Freire MO, Van Dyke TE. The mechanisms behind oral-systemic interactions. In: Glick M, ed. The Oral-Systemic Health Connection: A Guide to Patient Care. Chicago, IL: Quintessence; 2014:Chapter 5, 103-119.
Leishman SJ, Do HL, Ford PJ. Cardiovascular disease and the role of oral bacteria. J Oral Microbiol. 2010; 2. doi: 10.3402/jom.v2i0.5781.
The research, published in Alzheimer’s Research & Therapy, looked at more than 25,000 people to examine whether patients age 50 or older with severe gum disease – also called ‘chronic periodontitis’ – had an increased risk of developing Alzheimer’s disease.
Chang-Kai Chen (2017) ‘Association between chronic periodontitis and the risk of Alzheimer’s disease: a retrospective, population-based, matched-cohort study’, Alzheimer’s Research & Therapy, 9:56 https://doi.org/10.1186/s13195-017-0282-6
Periodontal diseases are mainly the result of infections and inflammation of the gums and bone that surround and support the teeth. In its early stage, called gingivitis, the gums can become swollen and red, and they may bleed.
A recent CDC report1 provides the following data related to prevalence of periodontitis in the U.S.:
- 47.2% of adults aged 30 years and older have some form of periodontal disease.
- Periodontal disease increases with age, 70.1% of adults 65 years and older have periodontal disease.
- This condition is more common in men than women (56.4% vs 38.4%), those living below the federal poverty level (65.4%), those with less than a high school education (66.9%), and current smokers (64.2%)
Periodontal disease, or gum disease, has two stages. The first stage is called gingivitis which can be hard to identify without testing. Unchecked and untreated, these responsible pathogens and their toxins are left to infect and recede the gums as well as freely escape into the bloodstream. The second stage is called periodontitis. Hallmark symptoms of periodontitis include red, bleeding, and tender gums, loose teeth, bad breath, and gum recession, as well as high levels of escaping oral bacteria shown to significantly contribute to other systemic disease conditions.
There is much controversy over saying the disease can be cured. However, there is evidence supporting that, in some circumstances, it can be reversed to the point it is no longer detected. Evidence also shows you can heal and regrow gum tissue and close pocket depths with the right protocols. The key is identifying the pathogens and understanding what you are treating by testing every patient. Without testing, blanket treatments can be too aggressive in one way, cause unnecessary resistance, or could possibly not be aggressive enough. You can learn how to manage and even reverse this condition in either stage with proper home care and maintenance testing to track the progress.
- What stage gum disease do I have?
- Do I have bone loss?
- What are my treatment options?
- How long will treatment take?
- How long will my recovery take?
- How often should I have my teeth cleaned to maintain the results of gum disease treatment?
Purple Complex:
– Aggregatibacter Actinomycetemcomitans (AA)
Red Complex:
– Porphyromonas Gingivalis (Pg)
– Tannerella Forsythia (Tf)
– Treponema Denticola (Td)
Orange Complex:
– Prevotella Intermedia (Pi)
– Campylobacter Rectus (Cr)
– Fusobacterium Nucleatum (Fn)
– Fusobacterium Animalis (Fa)
Green Complex:
– Eikenella Corrodens (Ec)
Caries:
– Streptococcus Mutans (Sm)
– Streptococcus Sanguinis* (Ss)
Yeast:
– Candida Albicans (Ca)
*The presence of Streptococcus Sanguinis is associated with healthy plaque biofilm.
Gone unchecked, pathogens and their toxins can easily move through the bloodstream with far-reaching and catastrophic effects on items like the heart, arteries, and central nervous system.
Periodontal diseases are disease processes involving the periodontium, a term used to describe the supportive apparatus surrounding a tooth, which includes the gingival tissue, alveolar bone, cementum, and periodontal ligament. Gingivitis is the mildest form of periodontal disease and can be found in up to 90% of the population. It is a reactive condition that is reversible upon the improvement of oral hygiene. Periodontitis is when the periodontal condition has progressed beyond gingivitis into a chronic, destructive, irreversible inflammatory disease state. The bacteria then can penetrate deeper into the tissues and surrounding periodontium. This triggers a host response in an attempt to defend against the invading bacteria. However, during the process of protecting against the bacteria, the host defenses also lead to the destruction of the periodontium. Periodontitis leads to loss of attachment of the periodontium, which subsequently progresses to alveolar bone loss, potentially resulting in loss of the affected tooth.
According to the American Dental Hygienists’ Association (ADHA.org,) approximately, 95 % of Americans with diabetes also have periodontal disease, due in part to an increased susceptibility to infections.
Diabetes that is not controlled well leads to higher blood sugar (glucose) levels in the mouth fluids. This promotes the growth of bacteria that can cause gum disease. On the other hand, infections from untreated periodontal disease can cause the blood sugar to rise and make it harder to control diabetes.
Another factor, smoking, is harmful to oral health even for people without diabetes. But a person with diabetes who smokes is at a much greater risk for gum disease than a person who doesn’t have diabetes.