Supporting Scientific Research
& Educational Collateral
Supporting Scientific Research
& Educational Collateral
Hormone Saliva Testing
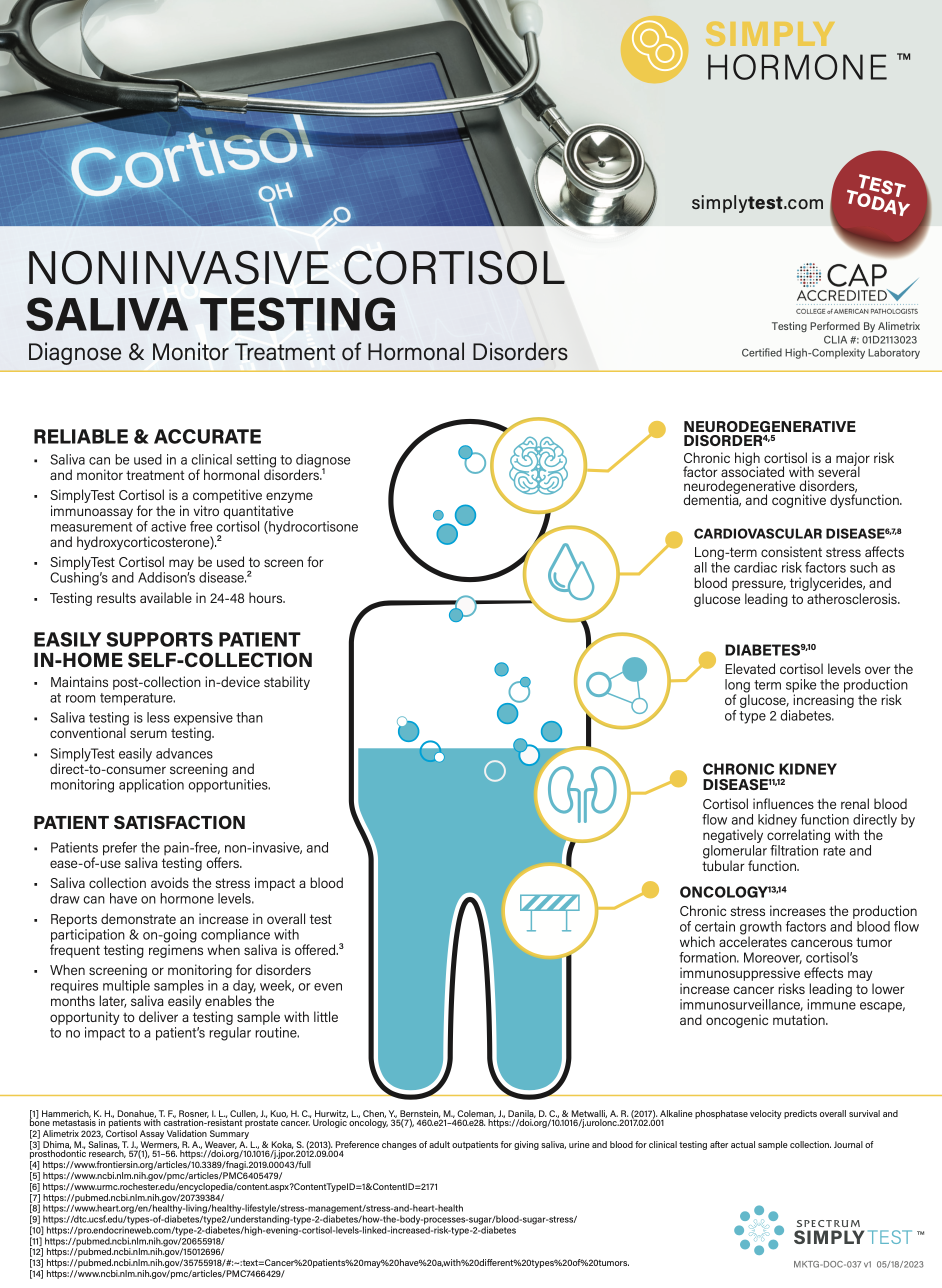
Noninvasive Cortisol Saliva Testing
(Download Provider Fact Sheet)
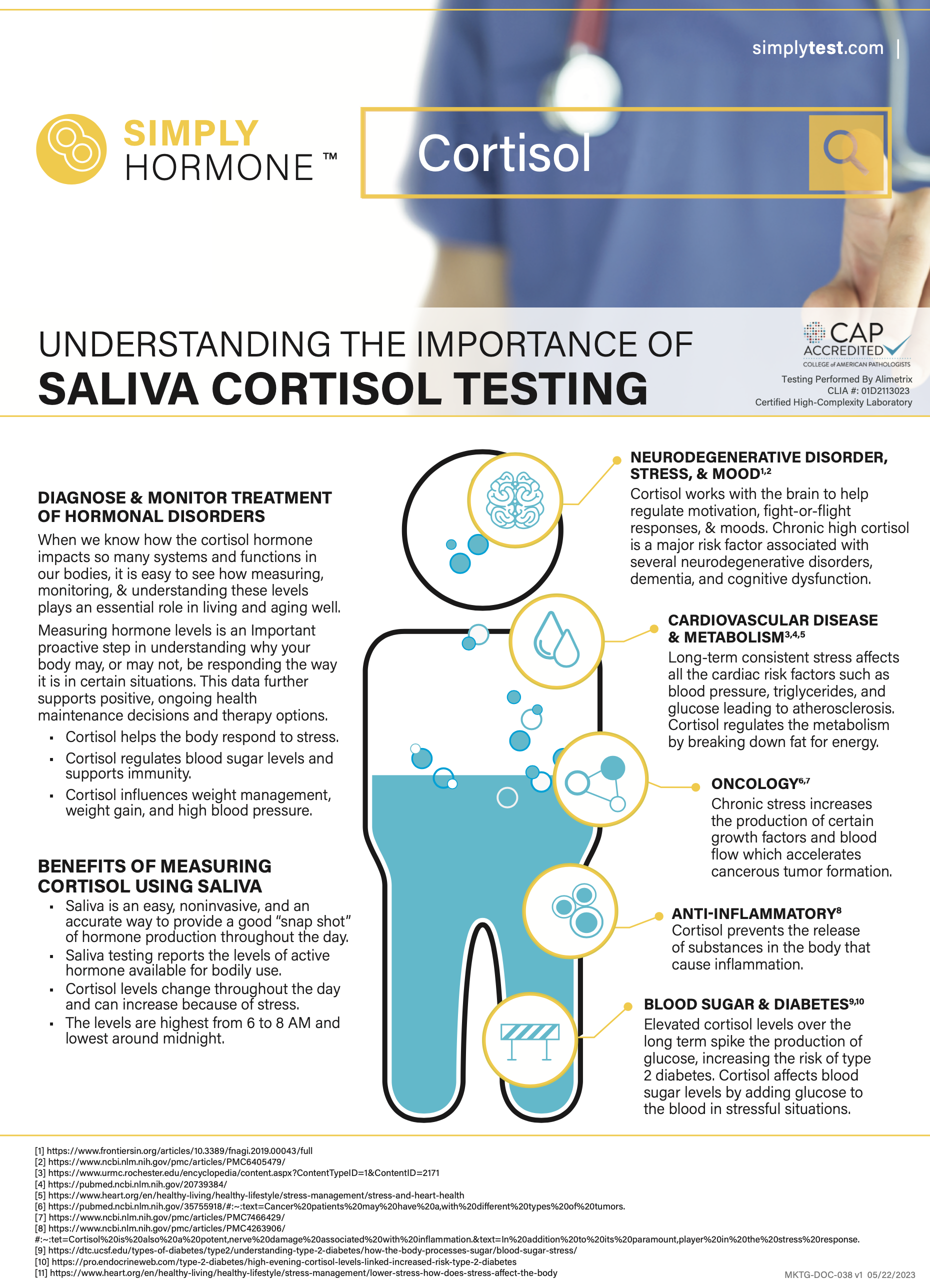
Noninvasive Cortisol Saliva Testing – Patient Education
(Download Patient Fact Sheet)
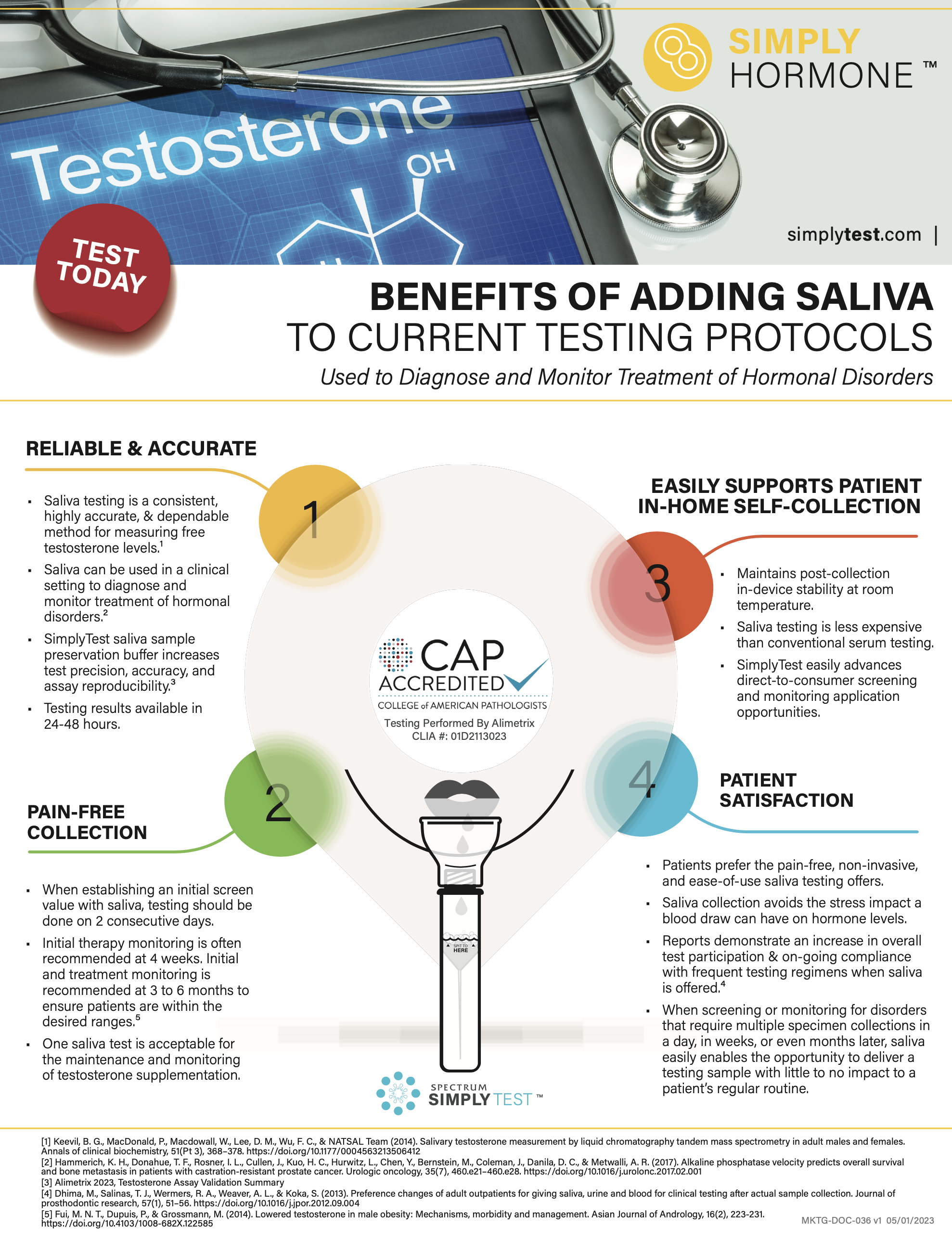
Noninvasive Testosterone Saliva Testing
(Download Provider Fact Sheet)
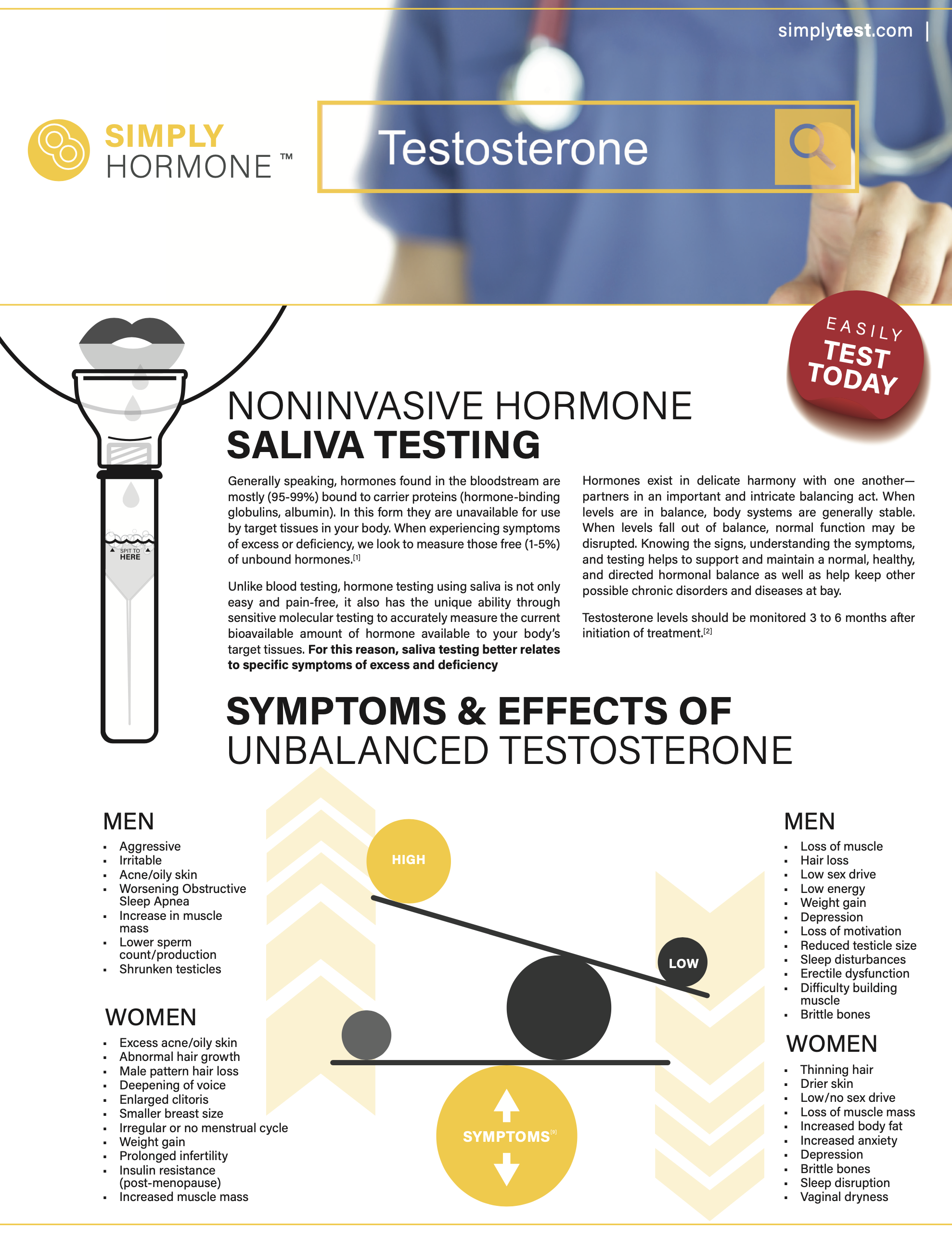
Noninvasive Testosterone Saliva Testing – Patient Education
(Download Patient Fact Sheet)
Noninvasive General Hormone Saliva Testing
(Download Fact Sheet)
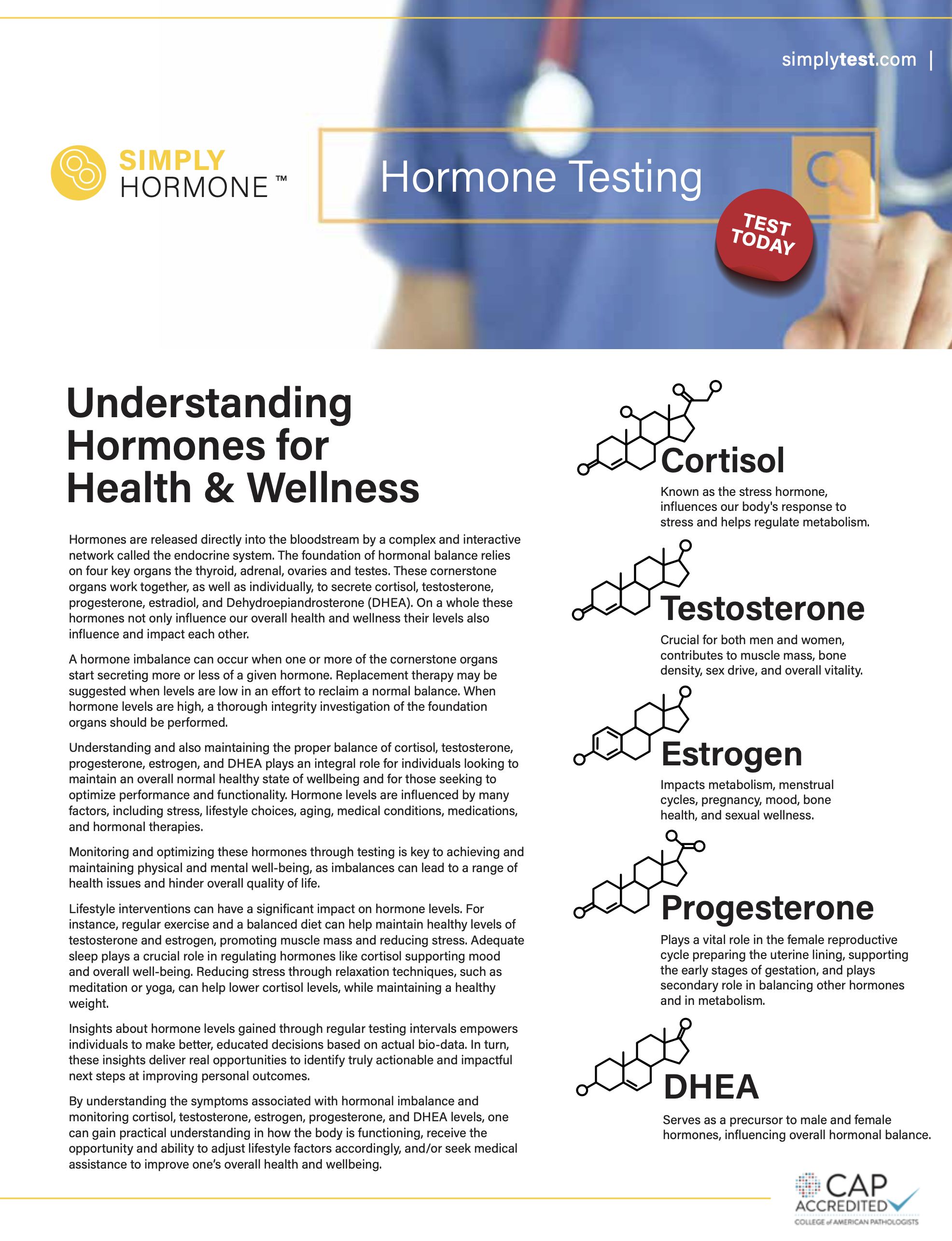
The Importance of Oral Hormone Screening
(Download White Paper)
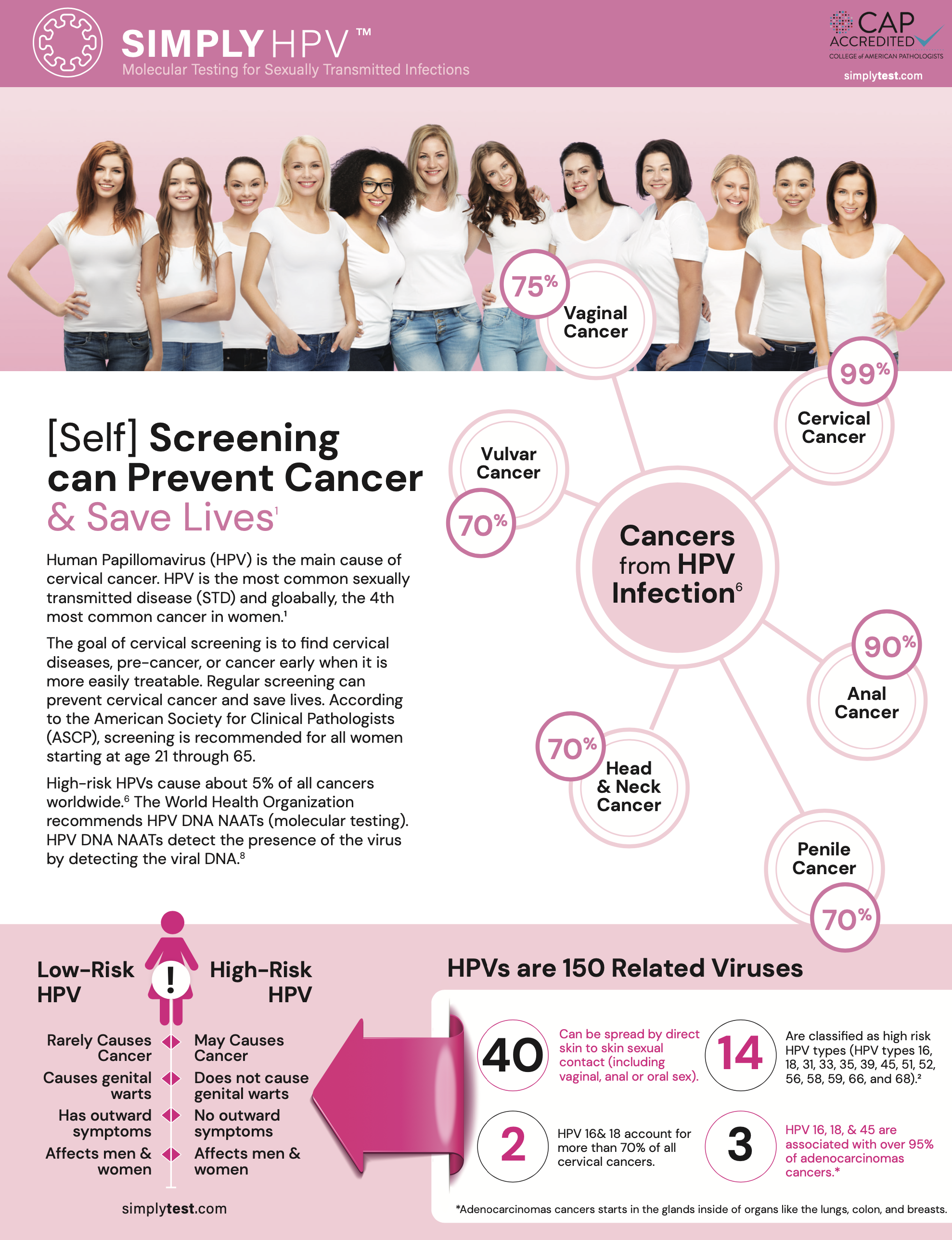
HPV Testing
Molecular HPV Testing Provider Fact Sheet
(Download Provider Fact Sheet)
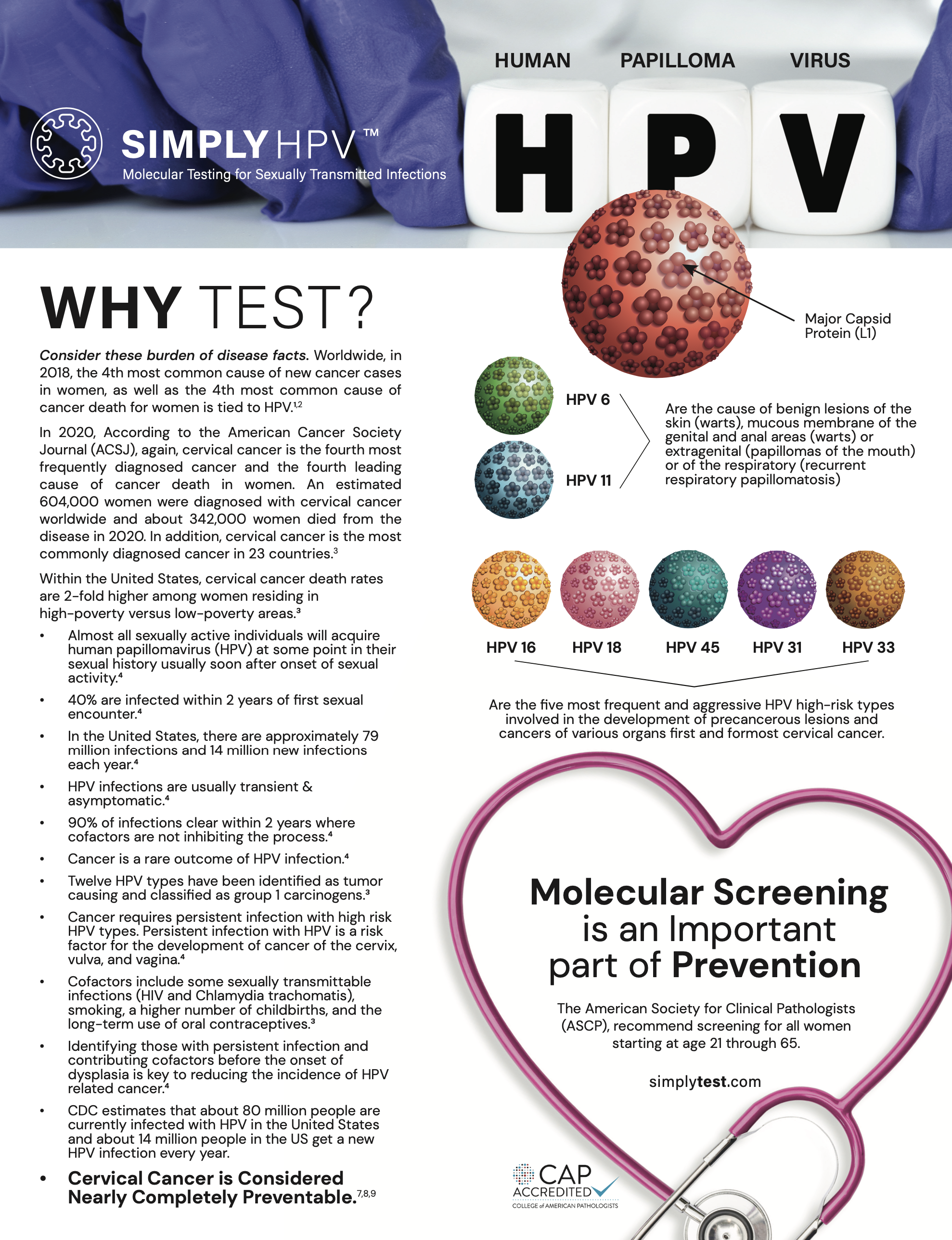
Understanding the Difference High-Risk Molecular HPV Testing – Patient Education
(Download Patient Fact Sheet)
The Importance of HPV Screening
(Download White Paper)
PERIO Testing
Evidence-Based Saliva Testing: Understanding the link between Oral Health and Systemic Disease
Periodontitis in Pregnant Women: A Possible Link to Adverse Pregnancy Outcomes.
Conclusion: Periodontal disease appears to be associated with adverse events in pregnancy due to the transport of biofilm bacteria into the bloodstream and into placental tissue; what would cause adverse events is the body’s immune response to infection. Periodontitis develops in 11% of pregnant women, and it is independently linked to severe complications during pregnancy such as preterm birth, low birth weight, and gestational diabetes. (Download PDF) or (view in published journal)
______
Can an Infection Hypothesis Explain the Beta Amyloid Hypothesis of Alzheimer’s Disease?
Conclusion: Many experimental data support the involvement of a polymicrobial community in the pathogenesis of AD. This “neurobiome” would be the backbone to support the new infection hypothesis of AD (Figure 1). This new hypothesis naturally incorporates the old amyloid hypothesis as Aβ is again on the center stage but as a puppet to infectious masters, rather than as a principal actor. This also throws a new light on neuroinflammation which precedes Aβ production and is not a consequence of it. So, in our view the question is not whether the microorganisms are the causative agents of AD but how and when they are inducing it. (Download PDF) or (view in published journal)
––––
Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors Brains
Conclusion: The findings of this study offer evidence that P. gingivalis and gingipains in the brain play a central role in the pathogenesis of AD, providing a new conceptual framework for disease treatment. Accordingly, we demonstrate the presence of P. gingivalis DNA and gingipain antigens in AD brains and show in vivo that oral administration of small-molecule gingipain inhibitors blocks gingipain-induced neurodegeneration, significantly reduces P. gingivalis load in the mouse brain, and significantly decreases the host AB1–42 response to P. gingivalis brain infection.
Our identification of gingipain antigens in the brains of individuals with AD and also with AD pathology but no diagnosis of dementia argues that brain infection with P. gingivalis is not a result of poor dental care following the onset of dementia or a consequence of late-stage disease, but is an early event that can explain the pathology found in middle-aged individuals before cognitive decline (60). We also demonstrate that P. gingivalis bacterial load can be detected in the CSF of clinical AD patients, providing further evidence of P. gingivalis infection of the CNS. (Download PDF) or (view in published journal)
–––––
The Role of the Oral Microbiota Related to Periodontal Diseases in Anxiety Mood and Trauma- and Stress-Related Disorders
Conclusion: There is an epidemiological association between diseases with altered oral microbiota such as periodontitis and anxiety, mood and trauma- and stress-related disorders, as reported by systematic reviews and meta-analyses. Less data are available for anxiety disorders and trauma-related disorders as compared to depression; however, the data suggest a role for the oral microbiota in these disorders. (Download PDF) or (view in published journal)
______
Periodontitis and Systemic Markers of Neurodegeneration: A Case–Control Study
Conclusion: Scientific rationale for the study: Peripheral inflammation is associated with high load of Aβ peptides in Alzheimer’s disease (AD). Periodontitis increases the risk of having cognitive decline; however, little is known on the potential role of periodontitis as a contributor to increased systemic concentrations of Aβ peptides in otherwise healthy individuals. Principal findings: Circulating Aβ peptides are elevated in periodontitis. A link between diagnosis of periodontitis and Aβ was observed, and enhanced systemic inflamma- tion could explain this relationship. Practical implications: Our results suggest that periodontitis via systemic inflammation could contribute to increased peripheral levels of Aβ peptides, which are key elements in the pathogenesis of AD. (Download PDF) or (view in published journal)
The Oral Fungal Mycobiome: Characteristics and Relation to Periodontitis in a Pilot Study.
Conclusion: In this first study comprehensively characterizing the oral mycobiome of adults with periodontal disease or good oral health, we observed trends of higher Candida abundance in participants with periodontal disease and participants with greater tooth loss. (Download PDF) or (view in published journal)
______
Candida Albicans Shields the Periodontal Killer Porphyromonas Gingivalis from Recognition by the Host Immune System and Supports the Bacterial Infection of Gingival Tissue.
Abstract: Candida albicans is a pathogenic fungus capable of switching its morphology between yeast-like cells and filamentous hyphae and can associate with bacteria to form mixed biofilms resistant to antibiotics. In these structures, the fungal milieu can play a protective function for bacteria as has recently been reported for C. albicans and a periodontal pathogen-Porphyromonas gingivalis. (Download PDF) or (view in published journal)
______
Association Between Candida Species and Periodontal Disease: A Systematic Review.
Abstract: Periodontal diseases result in the inflammation of the supporting structures of the teeth, thereby leading to attachment loss and bone loss. One of the main etiological factors responsible for this condition is the presence of subgingival biofilms, comprising microorganisms, namely bacteria, viruses, and fungi. Candida species is one of the fungi reported to be found in periodontal disease, which is suggestive of the presence of an association between these variables. The aim of this systematic review is to evaluate the association of Candida species with periodontal disease and determine the prevalence of these species in the patients affected with this disease. (Download PDF) or (view in published journal)

______
Yeast Diversity in the Oral Microbiota of Subjects with Periodontitis: Candida Albicans and Candida Dubliniensis Colonize the Periodontal Pockets.
Conclusion: The term periodontitis encompasses several polymicrobial infectious diseases of multifactorial etiology with chronic and aggressive forms. The objective of this investigation is to analyze the composition of the yeast microbiota present in the mucosa and subgingival sites of healthy individuals and patients with aggressive and chronic periodontitis. Patients with chronic periodontitis showed significant differences in relation to the other groups with respect to carrier status (69.2% versus 35.7% of healthy individuals; [chi(i)(2) test; p=0.014]), the total number of isolated colony forming units or CFU (mean and ranges 281.6 (0-6048) [K-W(2)=6.998; p=0.03]), the Simpson diversity index (I) in site b (I(b)=0.344 versus healthy subject and aggressive periodontitis where I=0 [multiple t-test comparisons with the Bonferronni correction, p<0.05]), and the species profile. Interestingly, in spite of the varied profiles of the species present in the mucosa of the three groups analyzed we noted that only C. albicans and C. dubliniensis were capable of colonizing the periodontal pockets in patients with chronic periodontitis, while only C. albicans was identified in the subgingiva of healthy individuals and patients with aggressive periodontitis. (Download PDF) or (view in published journal)
______
Occurrence of Candida albicans in Periodontitis -2021
Conclusion: Microbial-flora-associated periodontitis is very complex and has been continuously studied for many years. However, it should be emphasized that even if bacteria are considered as a primary agent in periodontal pathogenesis, other microorganisms, e.g., viruses and yeasts, are increasingly involved in the microbial etiology of periodontal diseases. Many studies showed an association between subgingival colonization by yeast subspecies, including Candida albicans, and the presence of severe periodontitis [6, 28]. Jarvensivu et al. [29] showed a prevalence of 16% in a population of 25 patients with chronic periodontitis. C. albicans remains the most common fungal pathogen found in patients with periodontitis [21, 22]. (Download PDF) or (view in published journal)

______
Association between Candida species and periodontal disease: A systematic review (PMID: 33628985) -2020
Conclusion: The aim of this systematic review was to evaluate the association of Candida species with periodontal disease and determine the prevalence of these species in the patients affected with this disease. The results of 21 studies were indicative of a positive association between Candida species and periodontal diseases. Accordingly, it was concluded that there is a strong association between the presence of Candida species and periodontal diseases (view in published journal)

A distinct Fusobacterium nucleatum clade dominates the colorectal cancer niche.
Fusobacterium nucleatum (Fn), a bacterium present in the human oral cavity and rarely found in the lower gastrointestinal tract of healthy individuals, is enriched in human colorectal cancer (CRC) tumours. High intratumoural Fn loads are associated with recurrence, metastases and poorer patient prognosis. Tumour-isolated strains predominantly belong to Fn subspecies animalis (Fa). (Download PDF) or (view in published journal)

Comparing the Cariogenic Species Streptococcus Sobrinus and S. Mutans on Whole Genome Level.
Conclusion: S. sobrinus can down-regulate the SpaA-mediated adherence to the pellicle. It has a smaller number of two-component signaling systems and bacteriocin-related genes than S. mutans, but all or even more immunity proteins. It lacks the central competence genes comC, comS, and comR. There are more genes coding for glucosyltransferases and a novel energy production pathway formed by lactate oxidase, which is not found in S. mutans. Both species show considerable differences in the regulation of fructan catabolism. However, both S. mutans and S. sobrinus share most of these traits and should therefore be considered as equally virulent with regard to dental caries. (Download PDF) or (view in published journal)

______
The Use of Probiotic Strains in Caries Prevention: A Systematic Review
Conclusion: The aim of this systematic review was to examine the role of the administration of probiotic strains in caries prevention. Mutans streptococci (MS) have been considered for a long time the major pathogens involved in caries development. Nevertheless, in recent years, it was described that the microflora on the tooth surface changes with caries lesion development, from a predominance of non-mutans streptococci and Actinomyces spp. to dominance of MS and other non-mutans bacteria, including lactobacilli and Bifidobacterium spp. [5]. The main goal for the use of probiotics in caries prevention is to replace and displace cariogenic bacteria, mainly mutans streptococci, with noncariogenic bacteria [13]. Results described by various research groups were encouraging [15–17,21–24,27,29–33,35,36], but the scientific evidence is still unclear and often not very high. (Download PDF) or (View study in published journal)
______
Dental Caries from a Molecular Microbiological Perspective
Conclusion: Dental caries results from an imbalance of the metabolic activity in the dental biofilm. This review highlights the fact that the principle molecular method, 16S rRNA sequencing, and subsequent population characterization for studying the diversity of the oral microbiome and the microbiota associated with caries is limited. New approaches, including the metagenomic, metatranscriptomic, metaproteomic, and metabolome analysis of oral biofilms, along with refined microbial sampling techniques, are required to improve our understanding of the ecology of caries. Such combined approaches will enable the genes expressed and the phenotypic characteristics of the biofilms at well-defined dental sites to be determined. Understanding the functioning, rather than just the composition of the microbial community, should be a high priority for caries microbiologists in the future. (Download PDF) or (View study in published journal)
______
The Role of Bacteria in the Caries Process: Ecological Perspectives
Conclusion: Our review of the literature supports the concept that dental caries is an endogenous disease, which is caused by a change from mutualistic symbiosis to parasitic symbiosis in the microbial ecosystem, i.e., a microbial shift from dynamic stability via acid-induced adaptation and selection to an aciduric stage, according to the extended ecological plaque hypothesis. In this hypothesis, the entire consortium of acidogenic/aciduric bacteria, not only the MS, contributes to the caries process—a view that is compatible with the mixed-bacteria ecological approach proposed by Kleinberg (2002). Acid production is the direct causative factor in the demineralization of tooth surfaces, but acid production is also an environmental determinant that influences both the phenotypic and genotypic properties of the oral microflora through acid-induced adaptation and selection. It is important to appreciate, however, that the enrichment of acidogenic/aciduric bacteria is a result of microbial acid formation during the caries processes—not the causative factor per se—and thus the removal of specific aciduric bacterial species such as the MS, through vaccination, gene therapy, or antimicrobial treatment, may not be an effective approach for long-term caries control. Rather, environmental control of the microflora should be achieved by avoiding acidification of the dental biofilm. Practical solutions to this strategy may include mechanical plaque control, reduction/substitution of the intake of sugary foods, and/or application of pH-neutralizing techniques such as saliva stimulation. (Download PDF) or (View article in published journal)
______
High-Risk Periodontal Pathogens Contribute to the Pathogenesis of Atherosclerosis
Abstract: Periodontal disease (PD) is generated by microorganisms. These microbes can enter the general circulation, causing a bacteraemia. Level A evidence supports that PD is independently associated with arterial disease. PD is a common chronic condition affecting the majority of Americans 30 years of age and older. Atherosclerosis remains the largest cause of death and disability. Studies indicate that the adverse cardiovascular effects from PD are due to a few putative or high-risk bacteria: Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola or Fusobacterium nucleatum. There are three accepted essential elements in the pathogenesis of atherosclerosis: lipoprotein serum concentration, endothelial permeability, and binding of lipoproteins in the arterial intima. There is scientific evidence that PD caused by the high-risk pathogens can influence the pathogenesis triad in an adverse manner. (Download PDF) or (view in published journal)

Inflammation in Periodontal Disease: Possible Link to Vascular Disease
Abstract: Inflammation is a well-organized protective response to pathogens and consists of immune cell recruitment into areas of infection. Inflammation either clears pathogens and gets resolved leading to tissue healing or remains predominantly unresolved triggering pathological processes in organs. Periodontal disease (PD) that is initiated by specific bacteria also triggers production of inflammatory mediators. These processes lead to loss of tissue structure and function. Reactive oxygen species and oxidative stress play a role in susceptibility to periodontal pathogenic bacterial infections. Periodontal inflammation is a risk factor for systemic inflammation and eventually cardiovascular disease (CVD). This review discusses the role of inflammation in PD and its two way association with other health conditions such as diabetes and CVD. (Download PDF) or (view in published journal)
Association Between Periodontal Disease and Atherosclerotic Cardiovascular Diseases: Revisited
Abstract: Atherosclerotic cardiovascular disease (ACVD) is an inflammatory disease of the coronary arteries associated with atheroma formation, which can cause disability and often death. Periodontitis is ranked as the sixth most prevalent disease affecting humans, affecting 740 million people worldwide. In the last few decades, researchers have focused on the effect of periodontal disease (PD) on cardiovascular disease. The aim of this review was to investigate the association between these two diseases. PD is a potential risk factor that may initiate the development, maturation, and instability of atheroma in the arteries. (Download PDF) or (view in published journal)
Assessment of Cardiovascular Risk in Women with Periodontal Diseases According to C-reactive Protein Levels
Abstract: Cardiovascular diseases (CVD) are highly prevalent non-communicable diseases worldwide. Periodontitis may act as a non-traditional cardiovascular risk (CVR) factor, linked by a low-grade systemic inflammation mediated by C-reactive protein (CRP). We aimed to assess the association between periodontal diseases and CVR in a group of adult women, based on serum high-sensitivity CRP (hs-CRP) levels; and secondly, to determine the association between serum and GCF CRP levels. (Download PDF) or (view in published journal)
Periopathogens in atherosclerotic plaques of patients with both cardiovascular disease and chronic periodontitis
Conclusion: This study demonstrated the presence of periopathogens in atherosclerotic plaques of patients with chronic periodontitis. More studies are required to ascertain the exact role of these periopathogens in atherosclerotic plaque formation. (Download PDF) or (view in published journal)
Apolipoprotein E gene polymorphisms in relation to chronic periodontitis, periodontopathic bacteria, and lipid levels
Conclusion: The aim of this study was to determine the possible effects of apolipoprotein E (ApoE) genotypes on the lipid levels in healthy people and patients with chronic periodontitis (CP) in relation to periodontopathic bacteria. (Download PDF) or (view in published journal)
The Link Between Different Infection Forms of Porphyromonas Gingivalis and Acute Myocardial Infarction: a Cross-Sectional Study.
Conclusion: The distant invasion and colonization of Pg were the risk factors of AMI. They also affected the severity of CHD, indicating that periodontitis severity and distant invasion of periodontal pathogens were related to CHD. The presence of Pg was likely able to drive systemic inflammation, suggesting that there was an inflammatory relationship between periodontitis and AMI. (Download PDF) or (view in published journal)
Periodontal disease is associated with the risk of Cardiovascular Disease Independent of Sex.
Conclusion: Cardiovascular disease is relatively common in patients with periodontal disease, and an increased risk of CVD is associated with periodontal disease independent of sex. Interventions targeting periodontal disease may be beneficial for CVD. (Download PDF) or (view in published journal)
Involvement of a Periodontal Pathogen, Porphyromonas Gingivalis on the Pathogenesis of Non-Alcoholic Fatty Liver Disease.
Conclusion: With the association between periodontal disease and the development of systemic diseases receiving increasing attention recently, we conducted this study to investigate the relationship between NAFLD and infection with Porphyromonas gingivalis (P. gingivalis), a major causative agent of periodontitis. The detection frequency of P. gingivalis in NAFLD patients was significantly higher than that in the non-NAFLD control subjects (46.7% vs. 21.7%, odds ratio: 3.16). In addition, the detection frequency of P. gingivalis in NASH patients was markedly higher than that in the non-NAFLD subjects (52.0%, odds ratio: 3.91). Most of the P. gingivalis fimbria detected in the NAFLD patients was of invasive genotypes, especially type II (50.0%). Infection of type II P. gingivalis on NAFLD model of mice accelerated the NAFLD progression. The non-surgical periodontal treatments on NAFLD patients carried out for 3 months ameliorated the liver function parameters, such as the serum levels of AST and ALT. (Download PDF) or (view in published journal)
______
High Prevalence of Periodontal Disease in Patients with NASH- Possible Association of Poor Dental Health with NASH Severity.
Conclusion: The present study suggests that NASH might be associated with periodontitis, irrespective of the intraoral presence of P.g. and A.a. Moreover, regular dental care utilization might mitigate the course of NASH, and patients should be reminded by their hepatologists of the importance of regular dental visits. 87.5% of NASH patients and 47% of controls suffered from moderate to severe periodontitis (p=0.01). Liver stiffness was significantly correlated with elevated PPD (p=0.02) and BOP (p=0.03). 34 % of the NASH patients did not make use of regular dental health care. In these patients, AST (p=0.04), MELD score (p<0.01), and liver stiffness (p=0.01) were significantly elevated compared to those who see a dentist regularly. The severity of NASH was not associated with the intraoral detection of P.g. and A.a. (Download PDF) or (view in published journal)

______
Herpesviruses and SARS-CoV-2: Viral Association with Oral Inflammatory Diseases – 2024
Conclusion: Viral infection of oral mucosal epithelia triggers an immune response that results in prolonged inflammation. While bacteria and fungi are the traditional focus of oral disease etiology, the contribution of viruses to oral pathologies is gaining increasing recognition. Viral infections of the oral cavity are common; however, our understanding of their role in oral disease pathobiology remains understudied. This review highlights the role of herpesviruses (dsDNA virus), and SARS-CoV-2 (ssRNA virus) in chronic inflammation-driven oral diseases, particularly gingivitis, periodontitis, peri-implantitis, and endodontic disease. While herpesviruses often establish latency in the oral mucosa, where they can reactivate and cause recurrent episodes of inflammation, growing evidence suggests that the periodontal pocket, gingival sulcus, and dental caries lesions serve as reservoirs for SARS-CoV-2 [11,136]. We provide evidence strongly supporting a relationship between HHV and SARS-CoV-2 and different oral inflammatory diseases. (Download PDF) or (View in published journal)
______
Periodontal Herpesviruses: Prevalence, Pathogenicity, Systemic Risk
Conclusion: An active herpesvirus infection of the periodontium exhibits site specificity, is a potent stimulant of cellular immunity, may cause upgrowth of periodontopathic bacteria and tends to be related to disease-active periodontitis. Pro-inflammatory cytokines induced by the herpesvirus infection may activate matrix metalloproteinases and osteoclasts, leading to breakdown of the tooth-supportive tissues. The notion that a co-infection of herpesviruses and specific bacteria causes periodontitis provides a plausible etiopathogenic explanation for the disease. Moreover, herpesvirus virions from periodontal sites may dislodge into saliva or enter the systemic circulation and cause diseases beyond the periodontium. (Download PDF) or (View in published journal)
______
Detection of Virus Herpes Simplex Type 1 in Patients with Chronic Periodontal Disease
Conclusion: Periodontal disease is an inflammatory-destructive condition of the supporting tissues of the teeth. Microorganisms found in the dental plaque were considered to be the primary local etiologic factor responsible for the periodontal destruction. This study analyzes the prevalence of herpes simplex virus type 1 (HSV-1) in the dental plaque (supra- and subgingival) of patients with chronic periodontal disease. Herpes simplex viruses type 1 are present in supragingival and subgingival dental plaque. (Download PDF) or (View in published journal)
______
Oral Lesions in Human Monkeypox Disease and their Management—a Scoping Review
Conclusion: Oral lesions may present as initial lesions of MPX suggesting that dentists and dental personnel should be aware of the nature of the disease. Clinicians must be alert to rashes resembling MPX lesions and distinguish MPX from herpetic and similar vesicular-bullous lesions for differential diagnosis. Symptomatic and supportive care for oral lesions is important. (Download PDF) or (view in published journal)

______
Understanding the Microbial Components of Periodontal Diseases and Periodontal Treatment-Induced Microbiological Shifts
Conclusion: Recent advances in laboratory identification techniques have contributed to a better understanding of the complexity of the oral microbiome in both health and disease. Periodontitis is now considered to be a multimicrobial inflammatory disease in which the various bacterial species within the dental biofilm are in a dysbiotic state and this imbalance favours the establishment of chronic inflammatory conditions and ultimately the destruction of tooth-supporting tissues. (Download PDF) or (view in published journal)
______
The Immunopathogenesis of Periodontal Disease
Conclusion: Treatment planning in periodontics, as with any disease, must be based on an understanding of the aetiology and pathogenesis of the disease. The aim of this review was to examine current understanding of the immunopathogenesis of chronic periodontitis with respect to its possible clinical implications in terms of treatment planning and risk assessment. The clinical implications of these observations can be seen in the fact that identification of Th1/Th2 and Treg/Th17 cytokine gene expression in the peripheral blood and salivary transcriptomes. (Download PDF) or (view in published journal)
______
Porphyromonas Gingivalis: Where do we stand in our battle against this oral pathogen?
Conclusion: Porphyromonas gingivalis is able to enhance oral dysbiosis, which is an imbalance in the beneficial commensal and periodontal pathogenic bacteria that induces chronic inflammation. To help medicinal chemists gain a better understanding of potentially promising scaffolds, this review provides an in-depth coverage of the various families of small molecules that have been investigated as potential anti-P. gingivalis agents, including novel families of compounds, repositioned drugs, as well as natural products. (Download PDF) or (View in published journal)
______
Periodontal disease as a risk factor for sporadic colorectal cancer: results from COLDENT study?
Conclusion: Accumulating evidence suggests periodontal pathogens are involved in colorectal carcinogenesis, indicating the need for high-quality epidemiological evidence linking periodontal disease (PD) and colorectal cancer (CRC). Results showed that the rate of new diagnosis of CRC in persons with a positive history of PD was 1.45 times higher than in those with a negative history of PD. Our results support the hypothesis of an association between PD and sporadic CRC risk. (Download PDF) or (View in published journal)
______
Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities?
Conclusion: Epidemiological, clinical interventional and experimental studies collectively offer sufficient evidence that periodontitis adversely impacts systemic health through biologically plausible mechanisms (Figs 2–5). Moreover, targeted therapies against specific periodontal pathogens (such as P. gingivalis and F. nucleatum) or the key virulence factors they produce (for example, gingipains and Fap2) might ameliorate specific comorbidities, such as Alzheimer disease and CRC. (Download PDF) or (View in published journal)
______
qPCR Detection and Quantification of Aggregatibacter actinomycetemcomitans and Other Periodontal Pathogens in Saliva and Gingival Crevicular Fluid among Periodontitis Patients Periodontitis Patients
Conclusion: The detection of special bacterial species in patients with periodontitis is considered useful for clinical diagnosis and treatment. Quantifying and differentiating these periodontal species from subgingival plaque and saliva samples showed a good potential as diagnostic markers for periodontal disease. (Download PDF) or (view in published journal)
______
Quantitative Molecular Detection of 19 Major Pathogens in the Interdental Biofilm of Periodontally Healthy Young Adults
Conclusion: In oral health, the interdental spaces are a real ecological niche for which the body has few or no alternative defenses and where the traditional daily methods for control by disrupting biofilm are not adequate. (Download PDF) or (view in published journal)
______
Periodontitis ADA Guidelines Evidence-Based Clinical Practice Guideline on the Nonsurgical Treatment of Chronic Periodontitis by Means of Scaling and Root Planing with or without Adjuncts. (ADA) Guidelines for Periodontal Therapy -American Academy of Periodontology Specific Antibiotics in the Treatment of Periodontitis Nonsurgical Treatment of Chronic Periodontitis by Scaling and Root Planing with or without Adjuncts: Clinical Practice Guideline (ADA) Systematic Review and Meta-Analysis on the Nonsurgical Treatment of Chronic Periodontitis by Means of Scaling and Root Planing with or without Adjuncts.
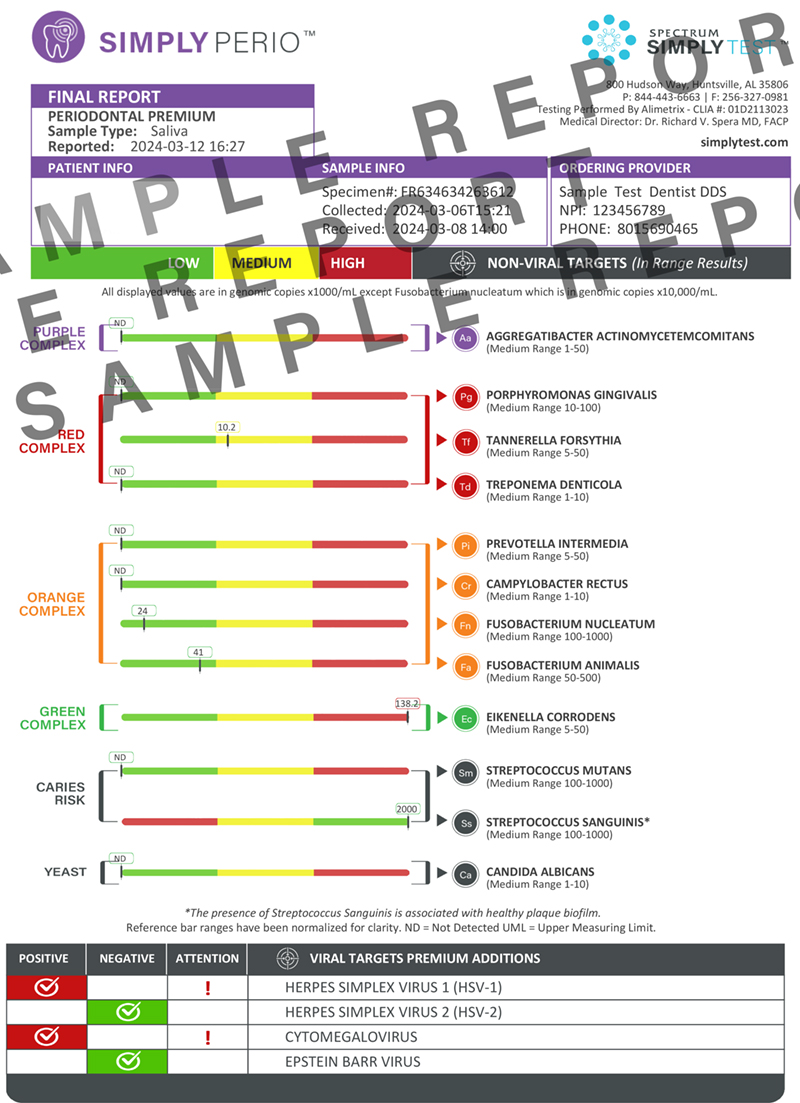
SimplyPERIO™ Sample Report
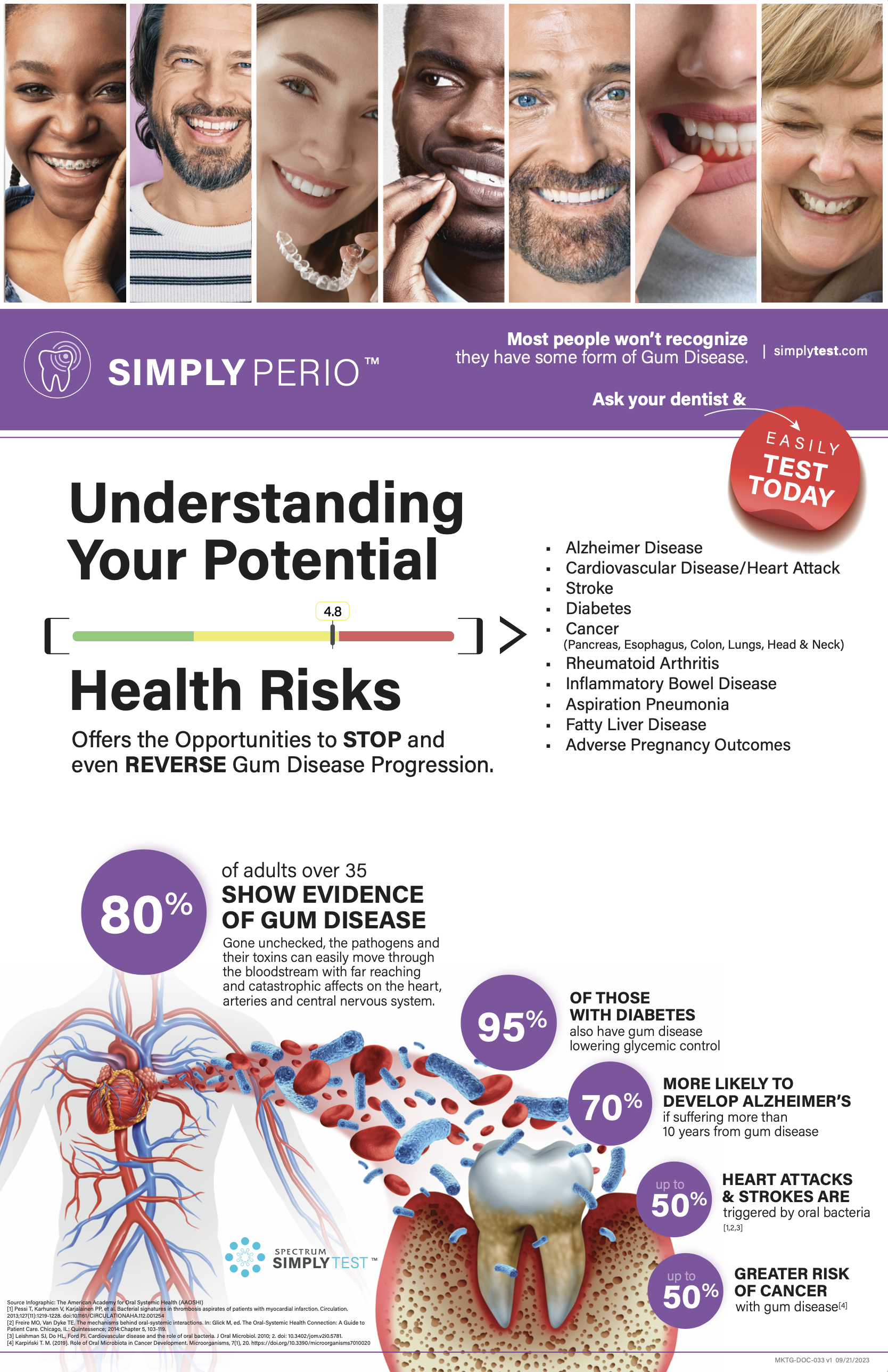
Understanding Your Potential Health Risks
(Download Poster)
You Share More Than You Think
(Download Patient Postcard)

_____________________________
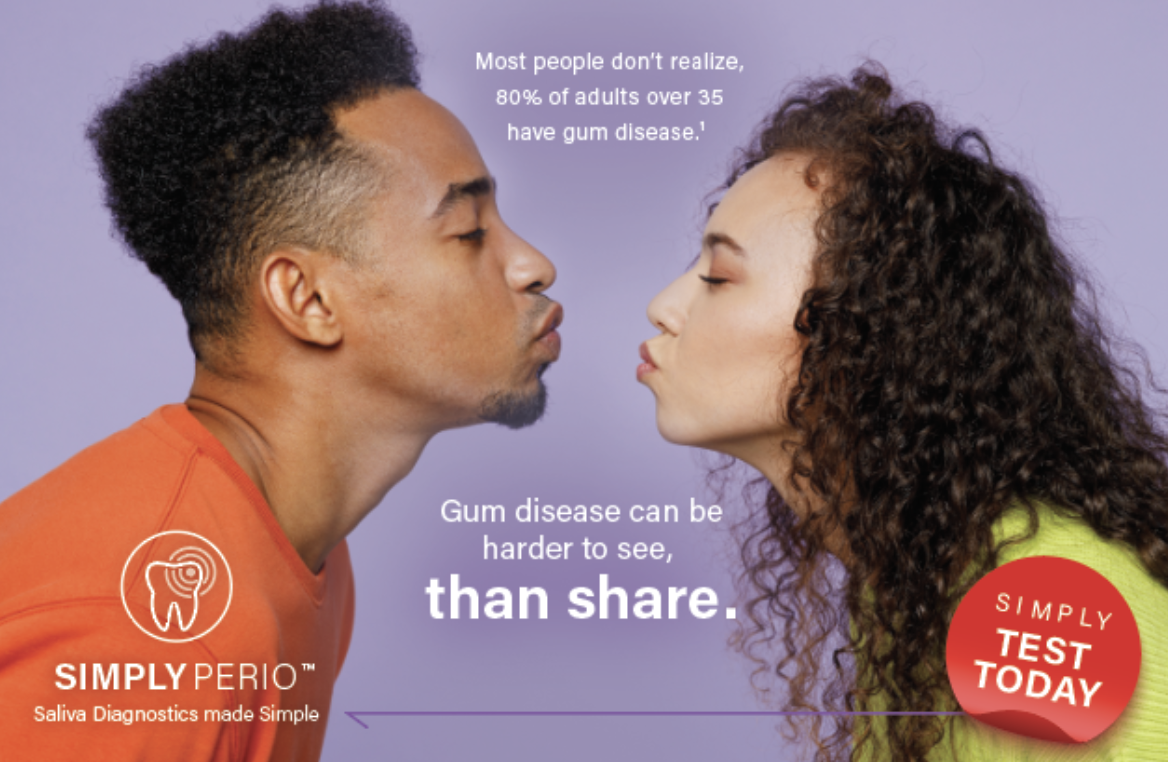
Perio Disease Can be Harder to See Than Share
(Download Patient Postcard)
______________________________
What if the Key to Better Health was Right Under Your Nose
(Download Patient Postcard)

Saliva Molecular Testing: Why Test, Who to Test, & How to Test Fact Sheet
(Download Fact Sheet)
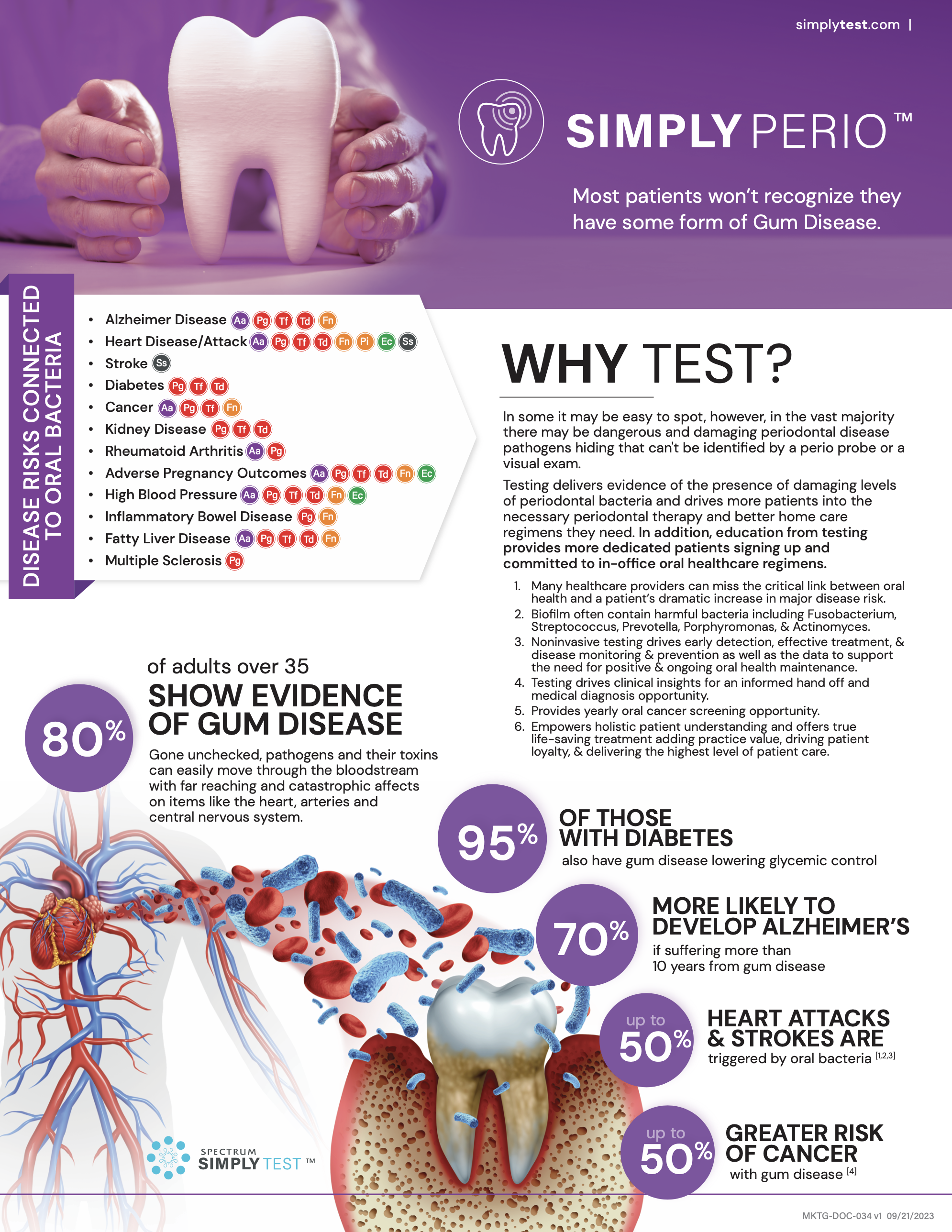
The Importance of Oral Periodontal Screening
(Download White Paper)

STI Testing
Industry-Leading, Simultaneous, and Most Comprehensive STI Molecular Detection
Why Test? Molecular STI Testing Provider Fact Sheet
(Download Provider Fact Sheet)
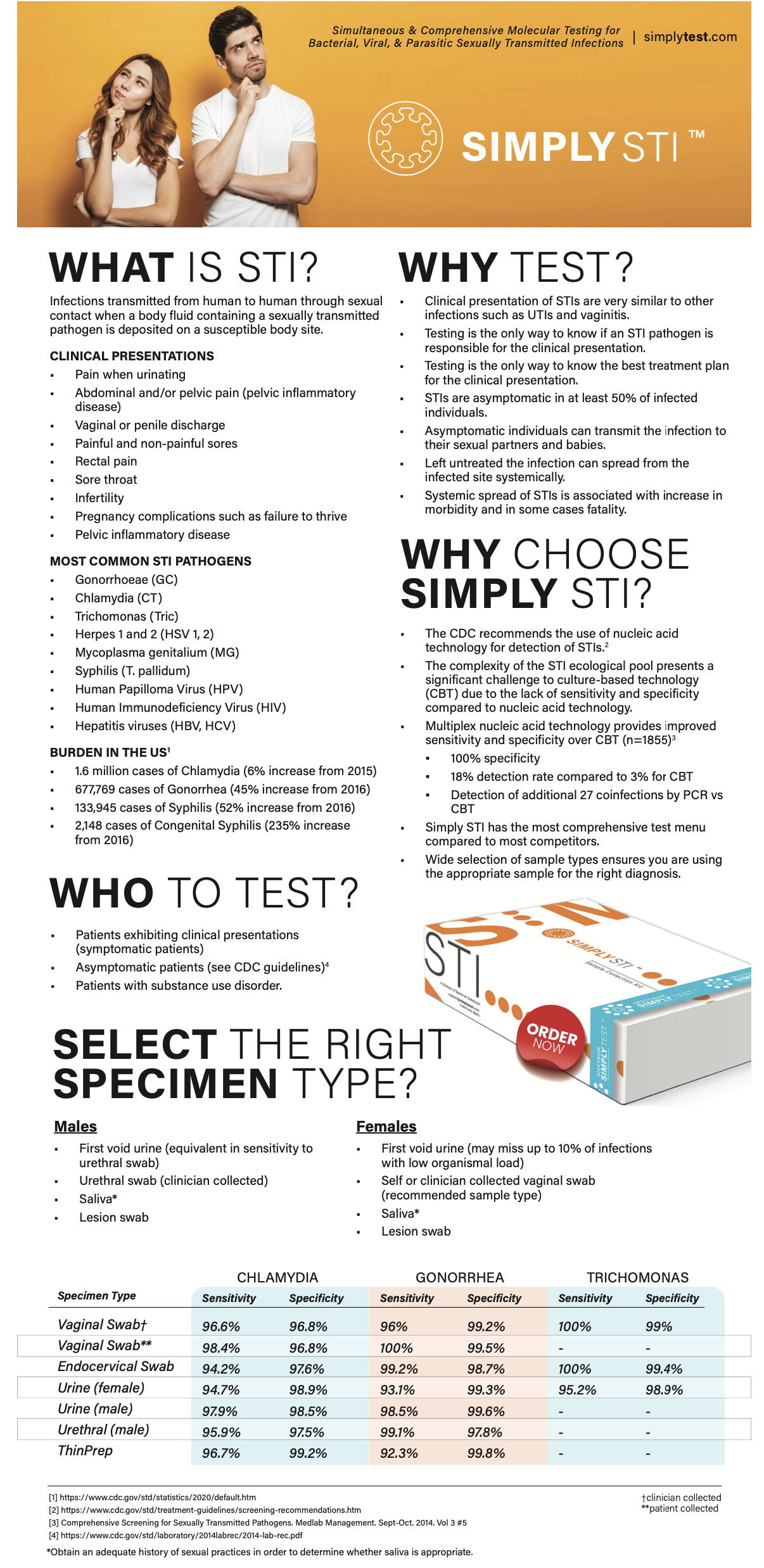
Understanding the Differences in STI Molecular Testing – Patient Education
(Download Patient Fact Sheet)

16″ x 20″ Complete STI Plus Pharmacy Poster
(Download Poster)

4″ x 6″ Complete STI Plus Test Pharmacy Info Card
(Download Info Card)

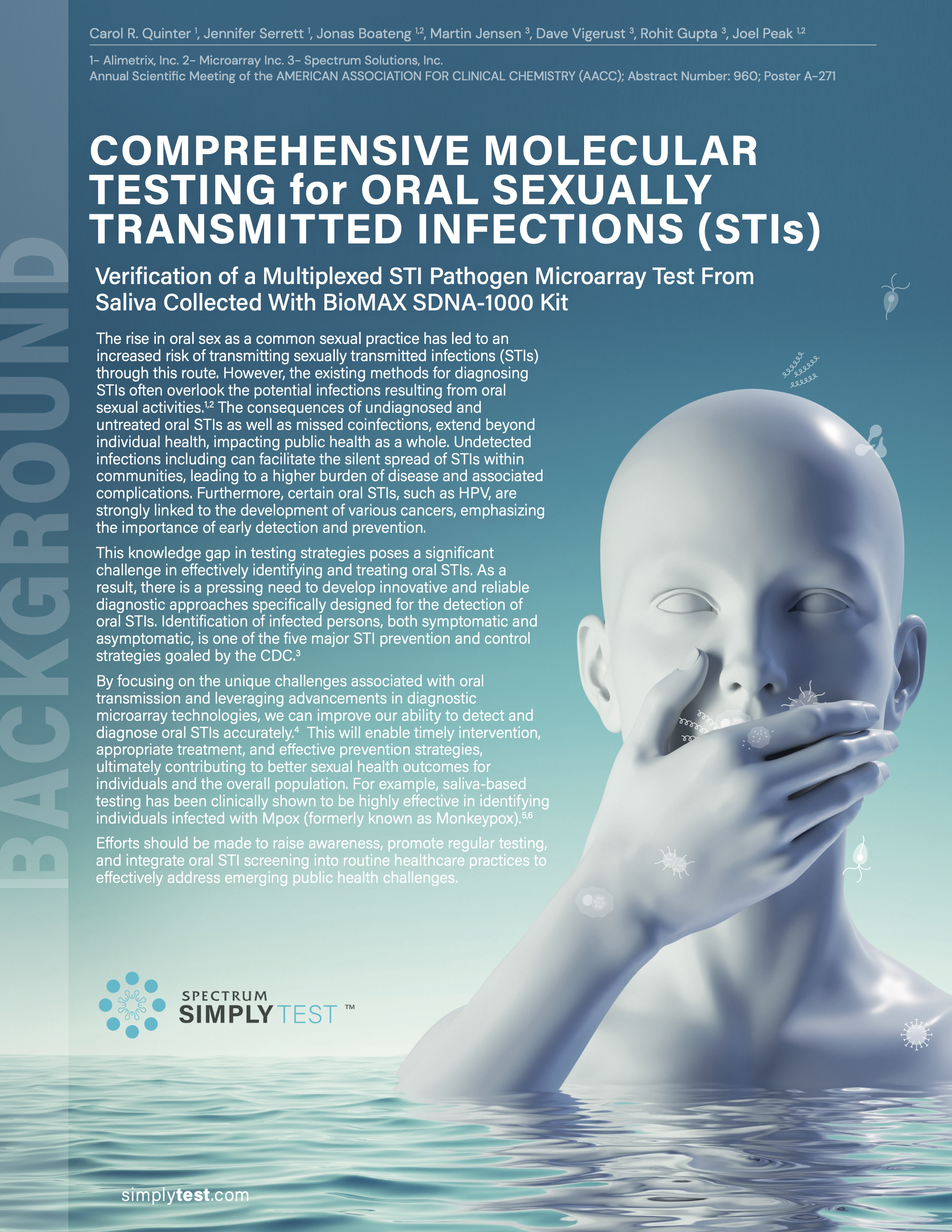
Comprehensive Molecular Testing for Oral Sexually Transmitted Infections (STIs) – SimplyTest™
AACC Poster Presentation
(Download Presentation)